“I must go forward where I have never been instead of backwards where I have.”
Winnie-the-Pooh
What I’ve realised over the last couple of weeks
What if after everything you’ve read on deliberate practice, you’re on board, but you’re still bothered by the uncertainty of where to start or how to continue practicing it?
That’s essentially what has been on my mind over the last couple of weeks. As I reflected on my own engagement with DP so far, that DP can be very challenging; can make someone want to throw in the towel, or put off getting into the ring in the first place.
These barriers can take many forms, as below, many of which have come up in my conversations with other people:
- Feeling overwhelmed coming to terms with changing old habits and what we have known (felt comfortable in).
- Feeling overwhelmed by which therapy/skill gap to address first.
- Feeling overwhelmed by trying to contain oneself to not work on too many skill gaps at once.
- Feeling overwhelmed trying to find the time to reflect on your practice in the first place.
- Feeling overwhelmed by Routine Outcome Measurement (ROM) data; how to interpret it and how to use it to inform what you need to improve.
- Feeling overwhelmed on which part of the DP system to start on, because DP cannot be prescribed as a step by step approach.
- Feeling overwhelmed on finding the time to start DP.
- Feeling overwhelmed on which ROM tools to use and how to implement them with clients.
- Feeling overwhelmed on finding a DP coach.
So that’s quite a few hurdles that can appear along that way and stop you in your tracks. I then started to think, based on my experiences so far, what insights could I offer someone struggling with the process. So if you’re feeling overwhelmed by these things, I have a suggestion, please take it with a grain of salt as it is based on my experiences and the goals I set for myself after reading Better Results. If any of the above challenges are making you procrastinate starting or continuing DP, it may be worth thinking about the following points and whether you could improve your work with clients in these areas:
- Using Routine Outcome Monitoring (ROM) E.g. the Outcome Rating Scale (ORS) and Session Rating Scale (SRS) to start gaining actionable feedback from clients. Chapter 6 of Better Results (page 97) talks about suggested spiels for introducing client’s to the ORS and SRS, while Chapter 9 (page 161) provides great pointers on the kinds of questions to use with client’s to increase the chance of gaining actionable feedback. ** This is where I started and it really helped provide clues on my other skill gaps to work on.
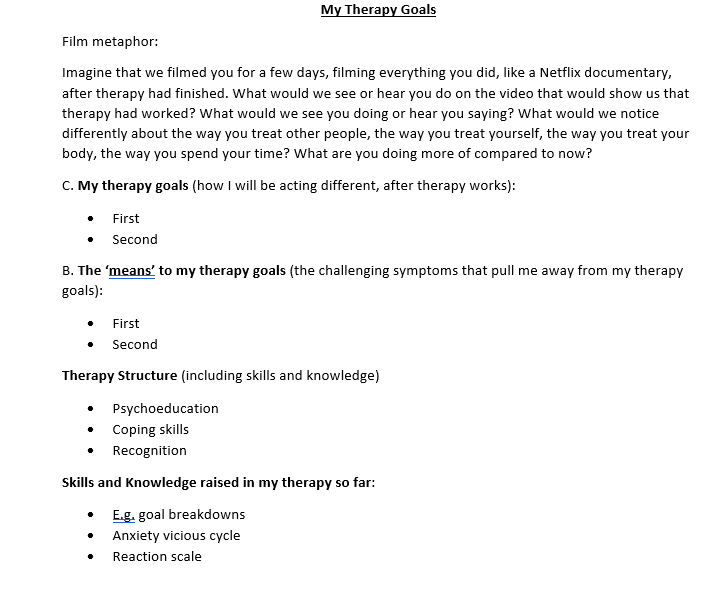
- Work on collaborative goal setting with clients – e.g. I focused on connecting with clients on what symptoms they wanted to work on and how they want their lives to be different from therapy as a result.
- Work on building the client alliance and therapeutic relationship – including empathy, congruence, caring, warmth, acceptance, positive regard, encouragement, affirmation and consensus building.
- Work on helping client’s create a conception of what to expect in therapy and a sense of hope (which is where I’m thinking of going next).
As Better Results posits, the above factors are known as the relational elements of therapy and are considered in research to be much more influential to therapy outcomes than treatment-specific factors, such as the treatment modality used. Better Results suggests that thinking about these relational elements can help one consider their strengths and weaknesses in these areas, to then inform a personalised professional development plan (page 96 and 97).
I stress importance on gaining actionable client feedback in sessions because this information can be used to work collaboratively with a client in their therapy, such as on goal setting, personally I see client feedback as like the guide to climbing Everest, without which it would be far easier to head in the wrong direction or get lost. These ideas are supported in Barry McInnes’ blog, where in a recent post he talks about a meta-analysis which suggests client feedback playing an important role in working collaboratively with clients; it’s an enjoyable read and I highly recommend Barry’s blog for anyone that wants to maintain a bridge between research and practice. He seems to have a knack for being on the forefront of therapy outcome research and does a great job translating it into interesting content.
A quote from Barry’s blog post: “Implementation of ROM and CFS is a process, not an event. The benefits are likely to be cumulative, as the Brattland study illustrates. Practitioners need to familiarise themselves with the process of introducing measures to clients, with interpreting and using the feedback from CFS, and using this feedback collaboratively with clients. We are not simply putting in place a new administrative. Rather, we’re learning a new set of skills.”
Now I know what I suggest may not be 100% in line with your skill deficits, but starting out this way may help build a sense of achievement and empowerment to gather momentum in DP – starting with small steps that feel manageable and then building up to bigger steps. Just like helping a depressed client to practice behavioural activation. Also, because these relational elements are considered to be amongst the most important factors in influencing treatment outcomes; there’s a reasonable chance that working on them will help your own therapeutic outcomes.
Sure this process can be a very scary and overwhelming one at times, but it can also feel very empowering and rewarding; over time creating a noticeable sense of self development. For instance, my goal setting originally just consisted of two things a) asking a client “what do you want to get out of therapy”, considering whatever they said to be the goal b) creating a symptom focused action plan.
Now so far after working on my goal setting, it now consists of three main elements:
- Helping clients understand how they want their lives to improve out of the therapy and what that will look like (our end goal).
- What symptoms they want to work on; the one’s that pull them away from a rich and meaningful life.
- Mapping out an action plan for working on these things, to then move closer to the rich and meaningful life.
Finally, I also remind myself that it’s ok to take things slow and make mistakes along the way, research is suggesting that DP takes years to get a grasp on, as it is skill development at the end of the day. Picking up a new hobby (I started bread baking from scratch) has helped me remember this, while also seeing others face similar challenges trying to improve their own skills -therapy related or not. Personally, I find inspiration watching others go through this; doing their best to improve.
I’m offering these thoughts on the back of something that Scott Miller said to me in an email recently – which is that we can’t know what challenges we will face in DP until we experience it. I’m aware that some of the challenges I have spoken about in this post can prevent someone engaging in DP in the first place. So if you have a fear that in starting out you might step the “wrong way” or you’re disappointed that your initial attempts have not been useful – remember that there is help and guidance out there, if you haven’t read the Better Results book I constantly mention, it is a great place to start as well. I’m hoping that sharing my experiences and these ideas might help someone to press on; every Adam Sandler needs their Rob Schneider.
If you need a few Rob Schneiders on your side – go to my resources page – and you’ll find plenty of groups to take part in with people to talk to about DP. Literally everyone I have reached out to so far has been very nice and accommodating to my thoughts and questions.
Case and point on how rewarding I have found this process – I recently noticed the importance and flow on effect of working on my goal setting. First, I could argue most of the clients I have had drop out over recent months could be largely attributed to a lack of therapy direction and goal setting in our sessions, though to be fair I can’t be sure. On top of this, it seems that the clients I have now where therapy goals are less clear; I’m more likely to engage in my over compensatory behaviours of overexplaining psychoed and homework. Where as with my newer clients, where goal setting has been more deliberate I have had less tendency to overexplain homework and keep to my planned SRS discussion time successfully at 10 minutes to the end.
What I’ve managed to do since my last post
Obviously, goal setting with clients is still my focus, I have continued the process I spoke about in my two most recent posts when it comes to goal setting. I have started to feel more natural in how I prompt clients to consider their goals and have been more often framing questions towards want they want to be moving towards/do more of/approaching as opposed to what they want to be doing less of. e.g. if you procrastinate less – what would you be doing more of instead?
This has helped my goal setting document, which I discuss with clients, turn into this (thanks to Russ Harris for the film metaphor which, which I modified slightly):
I didn’t get to have my 3rd coaching session, as I it was on the day of my 2nd COVID jab; which made me feel tired for the day, but I have continued with the sessions of solitary DP using LOVO. I’m starting to feel more comfortable with it now – I plan to do a video of how I use LOVO, which I’ll aim to have ready for my next post.
“Son, if you really want something in this life, you have to work for it. Now quiet! They’re about to announce the lottery numbers.”
Homer Simpson
Further thoughts on a system for session reflection
I thought I would finish up on something else, I was going to talk about this next time but I’ve decided to introduce it now – as next time I want to focus on the role of self-doubt in DP and some new scales that I’ve been lucky enough to get the opportunity to try thanks to NOVOPSYCH before they roll out . In this post at the start I briefly spoke about an idea to use the concept of schema coping styles in an attempt to notice and reflect on my safety behaviours in therapy sessions. I have decided to alter that idea slightly to instead reflect on DOTS from Acceptance and Commitment Therapy.
A good way to think about DOTS are as our natural human reactions to discomfort or distress when encountering something we cannot directly control (whether it be a situation, outcome, challenging thought or emotion, the past, the future, other people’s perceptions etc), the concept is like safety behaviours.
DOTS stands for:
– Distraction
– Opting out (avoidance)
– Thinking strategies (e.g. rumination)
– Substances/Self-Harm/Other Strategies.
Specifically, I’m going to see if noticing/reflecting on my use of DOTS as a therapist in a session will help me pick up on my skill gaps. For example, I may opt out reviewing with a client how their homework went from a previous session because I’m worried about whether they found it useful (which I cannot control). So therefore how I review homework with clients would be something to address. It’s not always easy to pick up what I’m trying to control exactly, so sometimes I just pick up the DOTS behaviour first and work backwards. My current hypothesis is that if I’m engaging in a DOTS behaviour then I’m close to one of my skill deficits; like a radar.
I even made a scale that I’m planning to use once a week, I’m thinking for 10 minutes just before a solitary DP session I could reflect on my sessions from the previous week, pick a notable session and score myself just like the ORS or SRS (what I made I just altered the SRS template):
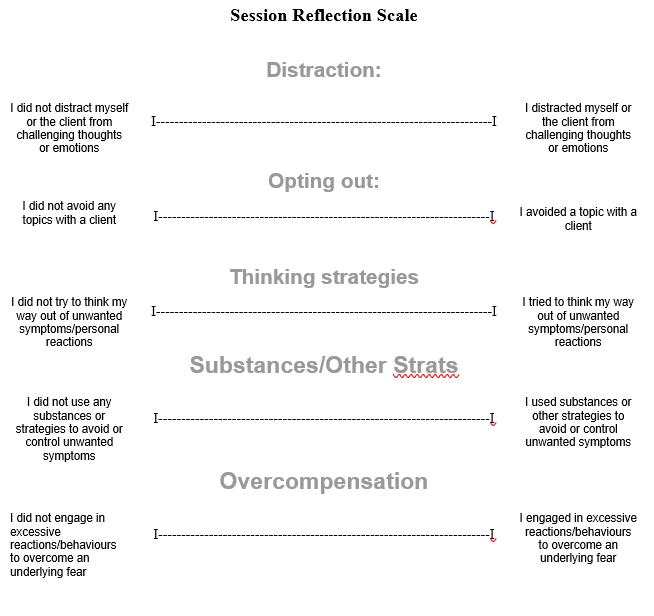
Lets see if this helps me to reflect on my sessions, to keep informing what I need to continue to work on, but to also keep my self-monitoring sharp. You’re welcome to use it if you want as well – just message me for a copy.
I hope that what I have spoken about today (and in my previous posts) helps someone reading this create a spark to keep at DP; some hope that it can be done, with an idea of what to expect – even though it’s not easy, I think it’s worth it.
Till next time and as always – thanks for reading.
2 responses to “Building expectations and hope for each other as therapists.”
[…] I added the following questions to the session reflection scale I previously […]
LikeLike
[…] right track, but Nathan helped me see a potential tweak to my approach. I was using a word document (as seen in this post) with clients to record their therapy goals and would dictate their goals into the document as they […]
LikeLike