When a client comes to see me, they say all they want is to get rid of their symptoms; their overwhelming stress, debilitating anxiety or pit of depression. They have tried everything to shake off what has become the ultimate tormentor in their life. Given all their power to problem solve and will these unwanted experiences away. When that doesn’t work they instead put their energy into getting away from their painful thoughts and emotions, either through distraction or suppression – or both. That’s until they get tired – too tired to keep up the battle alone. At this point desperation starts to seep in. That’s where I come in. I’m at the end of the line on the journey of having tried everything.

After building up the courage to book in the first session they are now in my waiting room completing the DASS-21, DSM cross cutting measure and C-NIP. With these tools the ball is already rolling and the client starts to engage. Once the session time hits, I bring the client into our therapy room. I direct the client to sit on the “big chair” (the couch) as I make final adjustments to kick off the session. I say hello and give them my name. I’ll often add a quick pleasantry; asking them how they went finding the place is usually my go to.
It’s from this point on, the starting line, that I interweave the core fabrics of how I do therapy. I start by explaining that the initial session “has a structure to it”. I tell them that I’ll begin by explaining the important admin (checking intake forms, explaining confidentiality and a quick demo on the booking portal). I’ll then explain the core focus of the first session and how that flows into the next sessions. Finally, towards the end of the session I’ll start to wrap things up and gauge with the client if anything was missing from the session or any changes need to be made with the therapy approach, which I “don’t take for granted”.
I like to explain the focus of the first session as “getting to know you and what’s brought you here”. I reassure clients new to therapy “that if you don’t know what to talk about, I’ll have a million questions for you anyway” and that “I won’t make you talk about what you don’t want to talk about”.

To give the purpose a more powerful picture I explain that therapy at this point is “like a puzzle – and that in the first session or two we’ll just be getting our puzzle pieces out of the box. Along the way we’ll start to piece things together. Once a picture starts to form we’ll figure out where to start in helping you cope with this puzzle – which will become our action plan in therapy – this gives us a crucial sense of direction. I add “that even in the first session I’ll do my best to provide you with something to go away with, but to strengthen that I need a reasonably deep understanding of what’s going on, otherwise I’ll just be shooting in the dark and that doesn’t do anyone any good”.
I then tell the client’s that “it’s not just the conversation I use to get to know you. I also use questionnaires. Two of the questionnaires I gave in the waiting area ask about symptoms. This is handy information because most client’s come in with symptoms they want to address, including things like stress depression and anxiety. However, from experience I’ve found that most new clients don’t just want to address symptoms…”
This is where I really start to hone in on presenting Routine Outcome Measurement (ROM) as part of the fabric of therapy.
I continue, “Most clients want to ensure their lives and wellbeing improve from therapy – so we need to go beyond just tackling symptoms”.
I can just about guarantee you that most of the time as soon as I say that I get a reassured nod and “Mhm” from the client. As if their saying – “that’s exactly what I’m looking for”.
Where the power comes from though, is that they didn’t know this is what they actually wanted – they came in focused on their symptoms. I’ve just validated what they really need and helped them realise it – therapy has already begun.
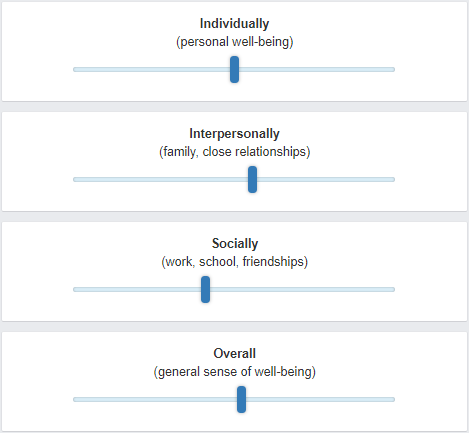
That’s where I introduce and take them through the Outcome Rating Scale (ORS) and paint this as the primary tool for tracking their well-being throughout the future sessions. As a gauge of if therapy is working or not, “because research demonstrates that a psychologists’ ability to just tell if you’re getting better or not… isn’t very good. This tool helps us get around that problem because the ORS gives a visual graph of how you’re going throughout therapy”.
For most clients, before they have even said anything of their story I already have a chunk of their buy in and for them we’re literally only just getting started.
This isn’t to say I use ROM with everyone, these days if clients tell me they have no interest in ROM however, I don’t try and convince them. I simply don’t use it – it’s not for everyone.
Using ROM in therapy can be a game-changer for clients. It’s not just about helping therapists understand what’s working or not working in therapy, the core purpose is to help clients see their progress, identify areas of focus, and get the most out of their therapy sessions.
When I use ROM with clients, I find that it helps me tailor therapy to a person’s unique needs. By using a tool like the ORS, which is quick and easy to use, I can get an overview of my client’s well-being and progress. But the most important thing is that my clients can see and feel the benefits of using ROM. If they don’t see how it helps them, they won’t engage with it effectively. That’s why I take the time to explain how ROM works and how it can benefit them.
The whole point of ROM is to benefit the client, not me. It’s an opportunity to change and improve the therapy approach when there’s evidence that the client isn’t experiencing the gains they are looking for. Further, if changing the therapy approach isn’t working, using ROM then makes it easier to identify if additional supports need to be considered, like bringing in other health professionals or even a change in therapist if things really are not working.
The bottom line is that ROM is a tool that can help clients get the most out of therapy. It’s not just about helping therapists track progress. It’s about giving clients the power to see their progress, to get the support they need to achieve their goals and have the life they deserve.
If you want to stay in the loop for future posts, then please feel free to sign up for our mailing list:
Deliberate practice at its core is a very simple system to follow. The challenge is that DP can become incredibly nuanced if you endeavour to deepen and strengthen your DP efforts. I believe a lot of people get put off by the nuances when they try to pick up DP. In order for DP to be successful, we first need to understand and concentrate on the foundations. The simpler those foundations can be presented, the easier it will be to engage with them; helping people to feel confident to give DP a go. DP is like mathematics, you can’t do complex maths unless you feel confident in the basics – which is why I suck at maths and avoid it. However the foundations of DP make sense to me and this is what has allowed me to create my own system of DP with increasing complexity over time.
A final note on why I’m writing these tips
2 responses to “DP TIP #3: Use Routine Outcome Measurement”
[…] Use Routine Outcome Measurement […]
LikeLike
[…] Use Routine Outcome Measurement […]
LikeLike